Wellness Recovery Action Plan (WRAP) Case Study
Info: 7628 words (31 pages) Dissertation
Published: 9th Dec 2019
Tagged: NursingHealth and Social Care
WELLNESS RECOVERY ACTION PLAN (WRAP)
Recovery is a principal component to a successful mental health services fit for the twenty first century and the key role of recovery focus services cannot be over-emphasized. This essay will highlight the importance of recovery; explore the conception and history of The Wellness Recovery Action Plan (WRAP); discuss a background information and assessment of a patient, various assessment tools to be used with the patient including risk assessment, symptom and rating scales; analyse the WRAP plan for the patient, justifying its risk assessment and plan; and finally discuss patient plan of care and its planning and implementation of the patient care. The Nursing and Midwifery Council (NMC) code of professional conduct directs that patient’s confidentiality and privacy should always be protected (NMC, 2015). As a result, the patient and the trust would be protected naming patient Ms Jones.
Recovery embodies the merging of various ideas including self-empowerment, personal management, rights of disability, social integration and therapy, and is undoubtedly one of the vital new focus for mental health services with support patients, mental health policy makers and other global mental health stake holders (South London and Maudsley NHS Foundation Trust , 2010).
Several authors have defined term ‘recovery’ but it remains a well contested one. Recovery has been seen as a continuing individual journey or process that is characterized by one’s own unique experience of mental disorder and the individuals understanding attached to this perception (Meehan, et al., 2008, p. 178; Provencher, et al., 2002; Kelly & Gamble, 2005, p. 246) with the possibility that the person is able to recover even if their mental disorder is not cured (Sydney West Area Health Service – Mental Health Network, 2008)
However, the definition by one of the intellectual founders of recovery management, Anthony (1993, p. 13), stands out and widely agreed:
“… a deeply personal, unique process of changing one’s attitudes, values, feelings goals, skills, and/or roles. It is a way of living a satisfying, hopeful and contributing life even with the limitations caused by illness. Recovery involves the development of new meaning and purpose in one’s life as one grows beyond the catastrophic effects of mental illness.”
According to Repper and Perkins (2003) and Slade (2009), Anthony’s description points to the fact that recovery is living a satisfied and enjoyable life which shift the focus of who has the power to define recovery from healthcare professionals to the individual. Shepherd and friends (2008) believe that mental health professionals should as a result sensitive and detach themselves from the allegation that they are trying to ‘take them over’. Nonetheless, for recovery to be effective, it requires professionals to know what it means so that together with the service user and other stake holders, appropriate interventions and support can be implemented (Shepherd, et al., 2008).
South London and Maudsley NHS Foundation Trust (2010)asserts that even that some people a recovery model, it is perhaps suitable to rather discuss recovery concepts and ideas because ‘a model’ gives the impression about an available recovery manual that a model would suggest that there is a Recovery manual somewhere that must be used to ‘fix’ people , but on the contrary, it is less so as recovery is about personalised approached.
Andresen and friends (2006) state that recovery is a process comprising elements of taking control and responsibility, finding and keeping hope, restoring a positive identity, having an optimistic life. This same view is support by South London and Maudsley NHS Foundation Trust (2010) who state that recover means living beyond illness without essentially accomplishing the eradication of the symptoms of illness; and also, the fact that recovery mean ‘social recovery’ does not necessarily mean clinical recovery known as symptoms and cure usually applied to people with long-term conditions or disabilities such as diabetes, asthma, arthritis. Moreover, recovery is a journey and therefore a period of illness does not equate to the fact that recovery has stopped, hence some people often say they in Recovery rather than Recovered. The support and involvement offered by mental health services is part of the journey of Recovery (South London and Maudsley NHS Foundation Trust , 2010).
Wilson and colleagues (2013) believe that recovery is an essential part of the path to healing and recovery from mental illness through which the person aims to regain autonomy, positive wellbeing, develop confidence, have the ability to manage their illness, and be optimistic about the future. Equally important to recovery from mental disorder is the need cope with the illness (Cook, 2005) through the use of recovery tools such as WRAP (The Wellness Recovery Action Plan) in the treatment and management of long term mental health issues (Copeland, 2005; Kennedy, et al., 2007)
Wellness Recovery Action Planning (WRAP) brainchild of Mary Ellen Copeland and others who have themselves experiences mental health problems and looking for ways to overcome their personal mental health problems and go on to enjoy a fulfil life, goals and aspirations (Copeland, 2005; National Health Service, 2017; WRAP, 2016). According to Copeland (2005) WRAP is a self-directed and recovery system designed to assist wellness, lessen symptoms, promote personal responsibility, or improve attribute concerning life. It educates individuals about how keep themselves well, to have the capacity to recognise and monitor symptoms, and the ability to use safe, individual skills, available support, early warning signs and other strategies to cope and mitigate symptoms
Copeland (2005) further describes WRAP as a tool that can help a person’s recovery and it is guided by principles that support the recovery plan. WRAP is a methodical way for checking health, times of being unwell and times when one is distressed and uncomfortable (National Health Service, 2017). WRAP helps the user determine their own simple and Safe Wellness Tool; list things they can do every day to stay well as much as possible; recognise triggers that cause upset, identify early warning signs and develop action plans for overcoming these moments (WRAP, 2016). WRAP has five key concepts that underpins effective recovery plan namely hope, education, personal responsibility, self-advocacy and support. These five principles are geared toward empowering people with mental health issues to take responsibility about getting well, staying well, make positive decisions about their life through learning from experiences and to also look outward in terms of supporting others to get well, by so doing they themselves feel better and enhances their own quality of life (WRAP, 2016; National Health Service, 2017). Copeland (2005) also stipulates that WRAP can also be used chronically mentally patients to manage their emotional and physical issues and also can help prevent or minimize the risk of relapse.
Argument exist about the conflict between objective and scientific nature of the medical model and the subjective and personally defined qualities that underpins recovery. On one hand, the medical model focuses on the on the illness and treatment based. It would be the main support for people but, is not sufficient. On the other hand, recovery model is about personalise person-centred holistic care which promotes strength and helps avoiding deterioration (Ralph et al.,200; May,2004; Allott et al.,2002) cited in Roberts and colleagues (2007).
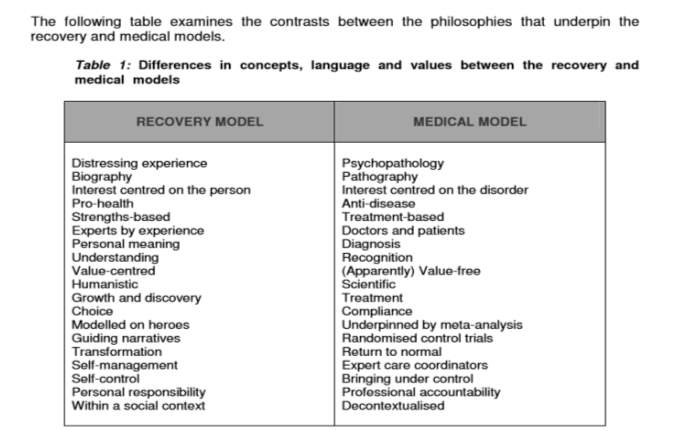 Source: Roberts and Wolfsom, 2004, p.40
Source: Roberts and Wolfsom, 2004, p.40
Patient Information
Ms Jones is a 41 years old single woman who lives in a two bedroom flat and works as a shop assistant in her community. She has been seeing her doctor for several months complaining of feeling low, she no longer enjoy work, lack of motivation, lack of sleep, loss of appetite and sometimes she experiences suicidal ideation when gets very unwell. After several tests, it was revealed she has no physical health problems. Ms Jones agreed agrees to be referred to the Psychiatrist by the GP for further assessment. She was diagnosed of major depression and was prescribe anti-depressant medication. Ms Jones was not concordant to her medication which makes her situation worse. More so, she becomes unwell and admitted that she has been having suicidal ideations. However, she mentions feeling labile mood, loneliness, isolated, stressed and anxious. She also mentions her history of depression which diagnose as stressed related in her early twenty’s. She also feels excluded from the community and even close neighbours. She has a daughter with previous partner but the relationship did not last. Ms Jones has never been in a meaningful relationship and she believes that men do not find her attractive. Ms Jones diagnosis correlates with NHS Choices (2016) and Mental Health Foundation (2017) as clinical depression. Ms Jones has also expressed concern that she does not feel well treated by the healthcare professionals as she feels they do not understand her condition and often look down on her and try to undermine her intelligence.
Assessment
During Ms Jones assessment, it was revealed that her family, friends, and the dog are her main strength, hope and support. Her day to day living was around her family and friends who’s supports her in all areas and it has serve as her coping mechanism, that is going out for tea, shopping, and walking the dog, she did mention feeling different and isolated from others. She also identifies that it rather becoming worse over the few months. she explains that she has not being in any meaningful relationship with men; the information gathered is to identify early warnings signs before things get worse.
The approach to the assessment is to inform intervention by identifying the clear target changes. Copeland (2005) stipulates WRAP has the capability to help sustain wellbeing, reduce symptoms, teaches how individuals can keep themselves properly, provide the ability to identify, monitor and use individual skills, support and other strategies to lesson symptoms, increase personal responsibility and improve the person’s quality of life. Brown and colleagues (2007) specifies that WRAP offers the opportunity to explore important ideals of recovery such as confidence, personal accountability, education, self-advocacy and support, and provides a planned progression for developing individualised WRAPs. This approach helps identifies the need of individual to motivates and empower them to takes control of their care and focus on their strength rather their weakness (Watkins, 2007).
The Daily maintenance
Daily maintenance plan is the most vital part of WRAP. This is where Ms Jones baseline is identified how she is when she is well (Bentley and Walsh, 2014). The daily day to day list activity and task to maintain her wellness. These are also the things that sustain her everyday living and if she does not them it shows she is unwell. She describes herself positive and optimistic, cheerful, and outgoing person when she well. she also mentioned that her to remaining well have a good sense of wellbeing family and the friends and they are her strength. According to the strength based approach model advises that, people have strengths within themselves that speeds up recovery, it argues that families could help as main source of building on these strengths, and plays greater roles in social relationship which promote hopefulness (Huiting, 2013)
(See appendices 1)
Triggers
These are the external factors that attribute to stressed, anxious and other negative symptoms which can affect the individuals. WRAP plan is to helps the individual identify the trigger and if can be avoided or helping them to manage (Center for Mental Health Services, 2013). Ms Jones identified her triggers as Financial hardship, Worries, Lack of support from friend and family anxiety, unpaid bills and the worse is when there are occasions like Christmas birthdays and anniversary because she forgets the dates or gets them mixed up and this further stress her the more. The plan is for Ms Jones seek help from her care coordinator and family help when she starts seeing these signs. Watkins (2007) argues receiving care and direction from health professionals, brings about collaboratively working with the individuals and families and other services to recognising triggers help recovery.
(See appendices 2)
Early Warning Signs
Copeland (1999) states that there are the signs that you need recognise and act to prevent the situation getting worse. When Ms Jones did mention about her early warning signs these would make her Isolate herself, withdrawal, feeling low, hopelessness, self-neglect inadequate sleep, Lack of motivation and loss of interest. When she starts feeling this way the plan agreed is to seek support from care coordinator and emergency help line soon as possible, take medication, notify the family, and friend, have adequate rest or relaxation, and breathing exercise. She said it can also increase suicidal thought since she has been diagnosed of major depression.
Care plan
Cambridgeshire and Peterborough NHS (2011) believes that the core of the clinical and therapeutic process of care planning is developing a relationship with the service user to structure their care plan. The action plan for Ms Jones was to contact the care coordinator to arrange an appointment with Cognitive Behaviour Therapist (CBT) to support and help her manage her problem by changing the way she behaves and thinks (NHS Choices, 2016). The concept behind CBT is the fact that one can be trapped in a vicious cycle by negative ideations, thoughts and moods due to the fact that our actions, thoughts, physical sensations and feelings are interlinked. CBT therefore helps the patient deal with overwhelming issues by breaking then down into little units to help deal with the current issue instead of focusing on the past (NHS Choices, 2016).
Also for Ms Jones would be encourages to structure her day and get involved in activities to help as distraction techniques. Family and friends to help get rid of things that can be used as weapon for self-harming such are any sharp items, be encourages to stay concordant to medication and to get enough sleep and other relaxation techniques. These plans will give Ms jones her some plan to follow and work towards to support and promote her recovery when this goes worse (Cambridgeshire and Peterborough NHS , 2011).
Crisis Plan: Nelson et al. (2014) states that WRAP identifies the unavoidability of crises in events by putting together a crisis intervention team. This view is also supported by Maller (2013) who believes that the initial thing to consider in an event is crisis planning. Maller is of the view that crisis plan in WRAP is subjective where he mentioned the overwhelming managing mechanism during crisis that can affect the capability to make right, safe and positive decisions. As shown In Ms Jones WRAP below, details of her symptoms showed that she is experiencing crisis is highlighted.
Post Crisis plan: Both Maller (2013) and Nelson Et al. (2014) again agree about the importance of tough times following crisis. Post crisis plan may include the support for Ms Jones to start a normal daily routine back at home (Nelson, et al., 2014), if she was if she was, for instance, detained under section 3 of the Mental Health Act (Legislation, 2007). Post crisis plan for Ms Jones in her WRAP could also include re-establishing relationships, paying her overdue bills and returning back to work. He WRAP planned may need to be amended to reflect her post crisis and it is best and effective this is done when she is in the process of coming out of her crisis (Nelson, et al., 2014)
Assessment tools justification
Depression is normally classified into the ICD-10 (International Classification of diseases, tenth edition) and the DSM-IV (Diagnostic and statistical manual of mental disorders, fourth edition) (American Psychiatric Association, 2000; World Health Organisation, 2010). These classifications are broken down in terms of the depression such as mild, moderate, major, bi-polar, postnatal, and seasonal affective disorder (SAD). According to Mental Health Foundation (2017), depression is described as major when it immensely affects an individual’s daily activities like happiness, eating, sleep, work, and relationships.
The most commonly used assessment tools for depression are Hamilton Depression Rating Scale (HDRS), Beck Depression Inventory (BDI), Patient Health Questionnaire (PHQ), Major Depression Inventory (MDI) (Medscape, 2017). In the case of Ms Jones, MDI is used for diagnosis and measurement of her depression because it falls in line with both DSM-IV major depression and ICD-10 moderate to severe depression criteria. The assessment tool is to determine the patterns of behaviour, mood and suicidal ideation which Ms Jones has reported has been going on for few months correlates the assertion by Medscape (2017) that symptoms should be present every day for the past two weeks. Depression Inventory tool which consists of 10 questions with a multiple-choices.
For depression to be diagnosed as major 1 or 2 either items in the 5 of 9 items in the list should be established. Ten items are listed in the diagnostic tool with the items given a value (0-5) which totals up to a theoretical score of 0 to 50. The limit is set to 26 for a depressive diagnosis to be deemed major or severe (see the table below 1) (Bech, et al., 2001). Furthermore, the level of the severity of depression is usually dichotomized into three by PQ-9 scores(Löwe, et al., 2004). PHQ-9 score of 6-10 is regards as moderate depression which would call for an intervention low-intensity in the form of a self-directed guide based on CBT. A PHQ-9 score of 15 and above indicate the presence of major depression which can be treated with antidepressant such as selective serotonin re-uptake inhibitors (SSIR) like fluoxetine and citalopram (Kroenke, et al., 2001). Furthermore, patient can also benefit from psychological treatments such as therapy, advice and counselling, and general information about depression, its management and treatment to assist deal with their depression as directed by NICE Guidelines (NICE, 2009).
Major Depression Inventory and rating scale score
| All of the time
5 |
Most of the time
4 |
Slightly more than half of the time
3 |
Slightly less than half of the time
2 |
Some of the time
1 |
At no time
0 |
|
| 1 Have you felt low in spirits or sad? | 5 | |||||
| 2 Have you lost interest in your daily activities? | 4 | |||||
| 3 Have you felt lacking in energy and strength? | 4 | |||||
| 4 Have you felt less self-confident? | 5 | |||||
| 5 Have you had a bad conscience of feelings of guilt? | 4 | |||||
| 6 Have you felt that life wasn’t worth living? | 5 | |||||
| 7 Have you had difficulty in concentrating, e.g., when reading the newspaper or watching television? | 4 | |||||
| 8a Have you felt very restless? | 4 | |||||
| 8b Have you felt subdued? | 5 | |||||
| 9 Have you had trouble sleeping at night? | 3 | |||||
| 10a Have you suffered from reduced appetite? | 0 | |||||
| 10b Have you suffered from increased appetite? | 3 |
Adopted from (Medscape, 2017)
Social exclusion can have adverse effect on individuals with mental health related issues such as building meaningful relationships, employment opportunities and have a good quality of life (NICE, 2017). SANE (2007) assert that it is obvious that stigma and discrimination still exist at the service delivery level. This view is highlighted by Del Veccio (2006) which stipulates that mental health professionals play a part in discrimination and stigma institutionalisation have surely born among the public’s impact that consumers are less than sordid humans (2006, p.646). Ms Jones has pointed out that she feels health professionals do not understand her condition and also feels looked down upon. To overcome this, education and training are options to discourage the continuation of these issue. The Royal College of Nursing (RCN) explains that health care practitioners have duty of care towards others in a certain way in a situation where it is reasonably foreseeable that the health professional might cause harm to people in their care through actions or omissions (RNC, 2017) while NICE (2017) advocates that health practitioners encourage social inclusion for patients by being respectful and sensitive to patients gender, sexual orientation, age, socioeconomic status, ethnic and religious backgrounds.
However, Del Veccio (2006) warns that in providing training staff training, caution needs to the used so that training does not rather perpetuate stigma and discrimination especially if the aim of the training is focused on the deficits of the consumer, and abandoning the resilience, abilities and strengths of those it serves. Rightly put, health care professionals are better place to strengthen low esteem of the patient by examining their value through the eyes of their disability Mancini and colleagues (2005, p. 51) and rather than assessing the treatment needs of the whole person, health care professionals should also focus on treating patients on the bases on their identified symptoms (Happell, 2008, p. 125). Health care practitioner’s awareness of duty of care and their ability to balance risk and coercion at the service delivery level can cause a barrier recovery (Mead & Copeland, 2000).
Reflection
The information gathered during the entire process indicate that Ms Jones has a history of Major depression which can be attributed to anything as she mentioned not having meaningful relations (Gibbs, 1998) reflective cycle states that all the stage is equally important these are context, thoughts, feelings, evaluation, analysis, reframe and future action. According to the (Nicol & Dosser, 2016)these stages continually help improve knowledge, understanding, learning and development of skills. However, Ms Jones had few things that would trigger her present situation looking at her history she did mention about depression in early twenty’s. I felt that 20year is a long time enough for to have plan in place to reduce her relapse and to charge of her care. However, WRAP is effective but can be time consuming which user may increase the stressing or the anxiousness of patient (Cook, et al., 2012). Overall, the assessment and treatment plan will support Ms Jones recovery and promote her well-being and autonomy.
In conclusion, this essay addresses recovery as principal element to a successful mental health services for the future and the would also play leading role in recovery focus services. Recovery from mental illness is the development of self-confidence, independence, ability to manage symptoms, to be optimistic about the future and going on the live a good quality of normal life. This essay explored by pointing out the importance of recovery by highlighting Wellness Recovery Action Plan (WRAP) which is an effective tool give mental health individuals enabling path for autonomy, improving on their quality of life, education and to having high individualised, exceptional process of changing their own attitudes and feelings, and setting goals (Anthony, 1993)and similarly help also them take control and responsibility, discover and keep hope, re-establishing a positive personal and social identity (Andresen, et al., 2006). Patient, Ms Jones, was identified to have depressive episode where the WRAP was used to plan her recovery. The essay showed that depression is classified into ICD-10 (International Classification of diseases, tenth edition) and DSM-IV (Diagnostic and statistical manual of mental disorders, fourth edition) (American Psychiatric Association, 2000; World Health Organisation, 2010). These are further broken down in terms of the depression being mild, moderate, major or severe. Ms Jones’ depression was diagnosed as severe because affects a person’s daily routines like being happy, appetite, sleep, education, work, and relationships then it is regarded as major. Health practitioner are directed to promote social inclusion by stamping out stigma and discrimination which can negatively affect people with mental health issue and consequently affect their full recovery (NICE, 2017)
References
American Psychiatric Association, 2000. Diagnostic and statistical manual of mental disorders (DSM-IVTR).. 4 ed. Washington DC: American Psychiatric Association.
Andresen, R., Caputi, P. & Oades, l., 2006. Stages of Recovery instrument: development of a measure of recovery from serious mental illness. Australian and New Zealand Journal of Psychiatry, Volume 40, p. 972–980.
Anthony, W., 1993. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal , Volume 16, pp. 11-23.
Bech, P. et al., 2001. he sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. Journal of affective disorders, 66(2), pp. 159-164.
Brown, W. & Kandirikirira, N., 2007. Recovering Mental Health in Scotland, s.l.: Scottish Recovery Netword.
Cambridgeshire and Peterborough NHS , 2011. Care Planning Guidance. Cambridge: NHS.
Center for Mental Health Services, 2013. Triggers: Disorders and issues. [Online]
Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3939995/
[Accessed 23 06 2017].
Cook, J. A., 2005. Patient-centred and consumer-directed mental health services. Prepared for the Institute of Medicine, Committee on Crossing the Quality Chasm–Adaptation to Mental Health and Addictive Disorders..
Copeland, M., 1999. Winning against Relapse: A Workbook of Action Plans for Recurring Health and Emotional Problems.. Oakland:: New Harbinger Publications, Inc..
Copeland, M., 2005. Wellness recovery action plan, Liverpool: Sefton Recovery Group.
Del Veccio, P., 2006. All we are saying is give people with mental illnesses a chance.. Psychiatric Services, 7(5), p. 57.
Happell, B., 2008. Determining the effectiveness of mental health services from a consumer perspective: Part 1: Enhancing recovery. International. Journal of Mental Health Nursing, Volume 17, pp. 116-122.
Huiting, X., 2013. Strength-Based approach for Mental Health Recovery. Iranian Journal of Psychiatry and Behavioural Sciences, 7(2), pp. 5-10.
Kelly, M. & Gamble, C., 2005. Exploring the concept of recovery in schizophrenia. Journal of Psychiatric and Mental Health Nursing, Volume 12, pp. 245-251.
Kennedy, A. et al., 2007. The effectiveness and cost effectiveness of a national lay-led self-care support programme for patients with long-term conditions: A pragmatic randomised controlled trial. Journal of Epidemiology and Community Health, 61(3), p. 254–26.
Kroenke, K., Spitzer, R. & Williams, J., 2001. The Phq‐9.. Journal of general internal medicine, 16(9), pp. 606-613.
Legislation, 2007. Mental Health Act 2007. [Online]
Available at: http://www.legislation.gov.uk/ukpga/2007/12/pdfs/ukpga_20070012_en.pdf
[Accessed 23 06 2017].
Löwe, B., Spitzer, R. & Gräfe, K., 2004. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. Journal of Affective Disorders, 78(2), pp. 131-140.
Maller, D., 2013. The Praeger handbook of community mental health practice.. California: Library of Congress.
Mancini, M. A., Hardiman, E. R. & Lawson, H. A., 2005. Making sense of it all: Consumer providers’ theories about factors facilitating and impeding recovery from psychiatric disabilities. Psychiatric Rehabilitation Journal, 29(1), pp. 48-55.
Mead, S. & Copeland, M. E., 2000. What recovery means to us: consumers’ perspectives.. Community Mental Health Journal, 36(3), pp. 315-328.
Medscape, 2017. Screening Tests for Depression. [Online]
Available at: http://emedicine.medscape.com/article/1859039-overview
[Accessed 23 06 2017].
Meehan, T. J., King, R. J., Beavis, P. H. & Robinson, J. D., 2008. Recovery-based practice: do we know what we mean or what we know?. Australian Journal of Psychiatry, 42(3), pp. 177-182.
Mental Health Foundation, 2017. Depression. [Online]
Available at: https://www.mentalhealth.org.uk/a-to-z/d/depression
[Accessed 22 06 2017].
Mental Health Foundation, 2017. Depression. [Online]
Available at: https://www.mentalhealth.org.uk/a-to-z/d/depression
[Accessed 08 04 2017].
National Health Service, 2017. Wellness Recovery Action Plan (WRAP). [Online]
Available at: http://www.southernhealth.nhs.uk/care/wrap/
[Accessed 20 06 2017].
Nelson, G., Kloos, B. & Ornelas, J., 2014. Community psychology and community mental health. New York: Oxford university press.
NHS Choices, 2016. Diagnosing clinical depression . [Online]
Available at: http://www.nhs.uk/Conditions/Depression/Pages/Diagnosis.aspx
[Accessed 22 06 2017].
NICE, 2009. Depression in adults: recognition and management.. [Online]
Available at: https://www.nice.org.uk/guidance/cg90/chapter/1-guidance
[Accessed 23 06 2017].
NICE, 2017. Guidance. [Online]
Available at: https://www.nice.org.uk/guidance/cg136/chapter/1-guidance
[Accessed 23 06 2017].
Provencher, H. L., Shery, R. G. & Mueser, K. T., 2002. The role of work in the recovery of persons with psychiatric disabilities. Psychiatric Rehabilitation Journal, 26(2), pp. 132-144.
Repper, J. & Perkins, R., 2003. Social inclusion and Recovery. London: Balliere Tindall.
RNC, 2017. Duty of CAre. [Online]
Available at: https://www.rcn.org.uk/get-help/rcn-advice/duty-of-care
[Accessed 22 06 2017].
Roberts, G., Davenport, S., Holloway, F. & Tattan, T., 2007. Enabling Recovery: The principles and practice of rehabilitation psychiatry. London: Gaskell.
SANE, 2007. Research Bulletin 4: Mental Illness and Stigma.. [Online]
Available at: https://www.sane.org/images/PDFs/SANE-Guide-to-Reducing-Stigma.pdf
[Accessed 21 06 2017].
Scottish Government, 2007. Better Health, Better Care: Action Plan.. [Online]
Available at: https://scottishrecovery.net/wp-content/uploads/2008/07/Realising-Recovery-Module3.pdf
[Accessed 05 06 2017].
Shepherd, G., Boardman, J. & Slade, M., 2008. Making REcovery a Reality. London: Sainsbury Centre for Mental Health.
Slade, M., 2009. Personal recovery and mental illness. A guide for mental health professionals.. Cambridge: Cambridge University .
South London and Maudsley NHS Foundation Trust , 2010. Recovery is for All , London: NHS Foundation Trust .
Sydney West Area Health Service – Mental Health Network, 2008. The Wellness Guide: A Resource to Support the Recovery Journey, s.l.: SWASHS.
Watkins, P., 2007. Recovery: a guide for mental health practitioners.. Philadelphia: Elsevier.
Wilson, J., Hutson, S. & Holston, E., 2013. Participant Satisfaction with Wellness Recovery Action Plan (WRAP). Issues in Mental Health Nursing, 34(12), pp. 846-854..
World Health Organisation, 2010. ICD-10. International Statistical Classification of Diseases and Related Problems. [Online]
Available at: http://www.who.int/classifications/icd/en/
[Accessed 23 06 2017].
WRAP, 2016. WRAP is…. [Online]
Available at: http://mentalhealthrecovery.com/wrap-is/
[Accessed 04 06 2017].
Appendix1
WELLNESS RECOVERY ACTION PLAN
WRAP
PERSONAL WORKBOOK
Name: Ms Jones
Age: 41
Address 21 Wynyard Court, Old brook, Milton Keynes. Mk6 3HD
Occupation: Shop Assistant
Telephone: 07448997645
Diagnosis: Major Depression
WELLNESS TOOLBOX
- In my experience, these are things that support my wellness – this works for me:
- Family and friends
- Going for leisure e.g. the saloon
- Walking my dog
- Relaxation and breathing exercise
- Sufficient rest and sleep
- Going to the cinema and theatre
- Shopping and eating out
- This is what carries a sense of meaning for me, what inspires me and reminds me of my values:
- My children and family
- My extended family supports
- My dog
- These are some things that I would like to try to see if they would support my wellness:
- Counselling and Cognitive Behaviour Therapist (CBT)
- Going to work
- Meeting my family and friends
Section 1
1. Daily Maintenance Plan
- My baseline: what am I like when I am well?
When I feel well, I am:
- Happy
- Cheerful
- Chatty
- Bright
- Shopping and cooking
- Relaxing
- Meaningful activities
- Completion of tasks
- Self-directed
- This is what I need to do for myself every day to keep myself feeling as well as possible:
- Talk to my family and friends
- Walk my dog
- Go to work
- Relaxing and breathing exercises
- To take my medication
- Eating healthy
- Baking
- This is what I need to do less often than every day, to keep my overall wellness and sense of wellbeing:
- Shopping weekly groceries
- Keep in touch with my parents
- Eating out with friends and family weekend
- Taking to my family and friends
- Going to the cinema
- These are the things that I know I need to do to sustain my wellness, but for some reason do not do them:
- Healthy eaten choices
- Daily exercise
- 8 glasses of water a day
- Adequate sleep
Section 2
2. Triggers
Recognition
Triggers are things that happen to us that are likely to set off a chain reaction of uncomfortable or unhelpful behaviours, thoughts or feelings…what triggers me?
- Anxiety
- Worries
- Financial hardship
- Unpaid bills
- Worries
- Non-concordance to my medication
- Lack of support from Friends and family
- Occasions e.g. birthday, anniversary
- Lack of support
Action Plan
What can I do about these triggers?
- Seek support from professional and GP
- Breathing exercise
- Seek family and friends support
- Involve in meaningful activity and enjoyable
- Walk my dog
- Take break from work if possible
Avoiding your triggers: What can I do to avoid or limit my exposure to things that trigger me?
- Concordance to medication
- Sufficient rest
- Going out with friends and family
- Keeping Dairy and daily planner
- Shopping
- Going to the cinema
- Going for short vacation break
- Exercise and walking the dog
- Eating and drinking health
Coping with triggers when they occur: What can I do when I am triggered to prevent things from getting worse?
- Support from Health professionals,
- GP
- Friends and family
- Engaging in meaningful activities
- Breathing and relaxation
- Going for a walk
Section 3.
Early warning signs are the subtle signs of changes in our thoughts or feelings or behaviour, which indicate that you may need to take action to avoid a worsening of your condition or situation
a. Recognition
What changes for me that are my early warning signs?
- Isolation and withdrawals
- Feeling low and hopelessness
- Self-neglect
- Inadequate sleep
- Lack of motivation and loss of interest
- Low dietary and fluid in take
- Non-concordance to medication
Action Plan
What can I do about this
What actions can I take when I recognise early warning signs?
- Seek support from care coordinators and emergency help.
- Take medication
- Family support and friends
- Walking your dog
- Relaxing and breathing exercise
- Adequate rest
- Good dietary and fluid intake
When things start getting worse
- Recognition
This is how I think, feel, and how I behave when the situation has become uncomfortable, serious or even dangerous:
- Withdrawal from family and friends
- Suicidal ideations/ self-harming
- Negative thoughts
- Low self esteem
- Self-neglect no interest in personal hygiene
- Sad
- Tearful and feeling hopelessness
- Low dietary or fluid take
- Staying indoors without coming out
- Kept myself
- Action Plan:
When things have progressed this far, caring for myself is my top priority. What can I do to reduce these difficult and unpleasant experiences, and prevent things getting worse?
- Support from family and friends
- Getting in touch with my care co-ordinator
- Get rid of things that can be used for to self-harm
- Concordant to medication
- Exercise and relaxation
- Sufficient sleep
- CBT therapy
Wellness Recovery Action Plan
This plan was made on 10/12/2016
And it takes over from any other plans with earlier dates.
Part 1. Remember what I am like when I am feeling well
When I am well I am:
- Positive
- Happy
- Joyful
- Optimistic
- Chatty
- Active
Part 2. When it gets too bad
When it gets too bad I
- Withdrawal
- Isolation
- Self-neglect
- Poor dietary intake
- Suicidal ideation
Part 3. Supporters
The list of people you like to take when things get worse
They can be family members, friends or health care professionals. You may want to name people for specific tasks; looking after the dog, like paying bills, etc
1
- Name: Lisa Turner sister 07799687557
- Support with paying bills
- Dealing with finance
- Making and keeping information on appointments.
2
- Name: Anna Clarke Auntie 07894561233
- Looking after the house
- Waking the dog looking after it
- Attending appointment with me
These two should decide on what is the best treatment option for me while consulting family.
- Name: Dr J Daniels, Psychiatric 07985249712
- Name: Dr P Parkins GP. 019088974561
- Name: Sue Webb Care Coordinator, 07811122209
I do not want the following people to be involved in any way in my treatment or care:
- My former partner Shaun O’Connell
Part 4. Medical Treatment and medication
- Name: Dr P Parkins GP. 019088974561
- Name: Sue Webb Care Coordinator, 07811122209
List medication you are currently taking and why you are taking them
- The of listed my medication in my charts can be useful.
List medication you would prefer to take if additional medication becomes necessary and why you choose those
- I prefer Fluoxetine I have less side effect on me and is clamming
List medications to be avoided and why
- Fluvoxamine
- Agitation
- Trouble in breathing
Part 5. Treatments
List other treatments that help reduce your symptoms and why they should be used:
- Having session with Psychologist
- Attending mindfulness
- CBT
List treatments you want to avoid and why:
- Group sessions
Part 8. Those who can support me to reduce symptoms or make me make things easier when I am in crises
The plan will be for me to stay at home and get support from community home treatment team. My will also like to get from my care co-ordinator and Psychiatric nurse
Part 9. If I am in danger
If my behaviour endangers me or other, I would like my supporters to:
- To the hospital
- Notify family and friend to step and take charge of all that include finances, bills and dog
Part 10. Inactivating the plan
Describe what positive changes indicate to your supporters that you are in control of things again, and that they no longer need to use this plan.
You will know it is safe to stop this plan when:
When a am well and stat taking care of my self
- Going to back to work
- Concordant to medication
- Keeping records of appointments and attending them
- Budgeting and pay bills.
What have you learned about yourself and others through this crisis?
- Recovery is ongoing process which required being positive and log team commitment
- necessary help and support from friends, family and professionals
Adapted from: (Working Together For Recovery, 2017)
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Health and Social Care"
Health and Social Care is the term used to describe care given to vulnerable people and those with medical conditions or suffering from ill health. Health and Social Care can be provided within the community, hospitals, and other related settings such as health centres.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




